Narcolepsy Symptoms: Cataplexy
Reviewed by: HU Medical Review Board | Last reviewed: November 2024 | Last updated: November 2024
Cataplexy is the sudden loss of muscle tone or muscle control in response to a strong emotion. A person with cataplexy may go limp and slump over or fall. They may be unable to move. Cataplexy can also be more subtle – a facial droop, or clumsiness. It may also be jaw weakness, grimacing, or tongue thrusting, especially in children. This symptom often is triggered by strong emotions such as joy or fear, a happy surprise, frustration, or intense stress.1,2
Only people with type 1 narcolepsy have cataplexy. Sometimes people with type 2 narcolepsy, or narcolepsy without cataplexy, go on to develop type 1 narcolepsy. When this happens, doctors believe the person likely had type 1 all along. Their orexin levels finally dropped enough for cataplexy to develop. Orexin is a hormone that plays a role in the sleep/wake cycle.1,3
How common is cataplexy with narcolepsy?
Cataplexy is the first symptom to appear in 1 out of 10 cases of narcolepsy. Some people may have only a few cataplexy attacks in their whole life. Others may have many attacks each day.1,2
About 70 percent of people with narcolepsy also have cataplexy. Cataplexy can develop weeks or sometimes years after daytime sleepiness begins in people. It rarely occurs in any other condition besides narcolepsy.2-4
What happens during cataplexy?
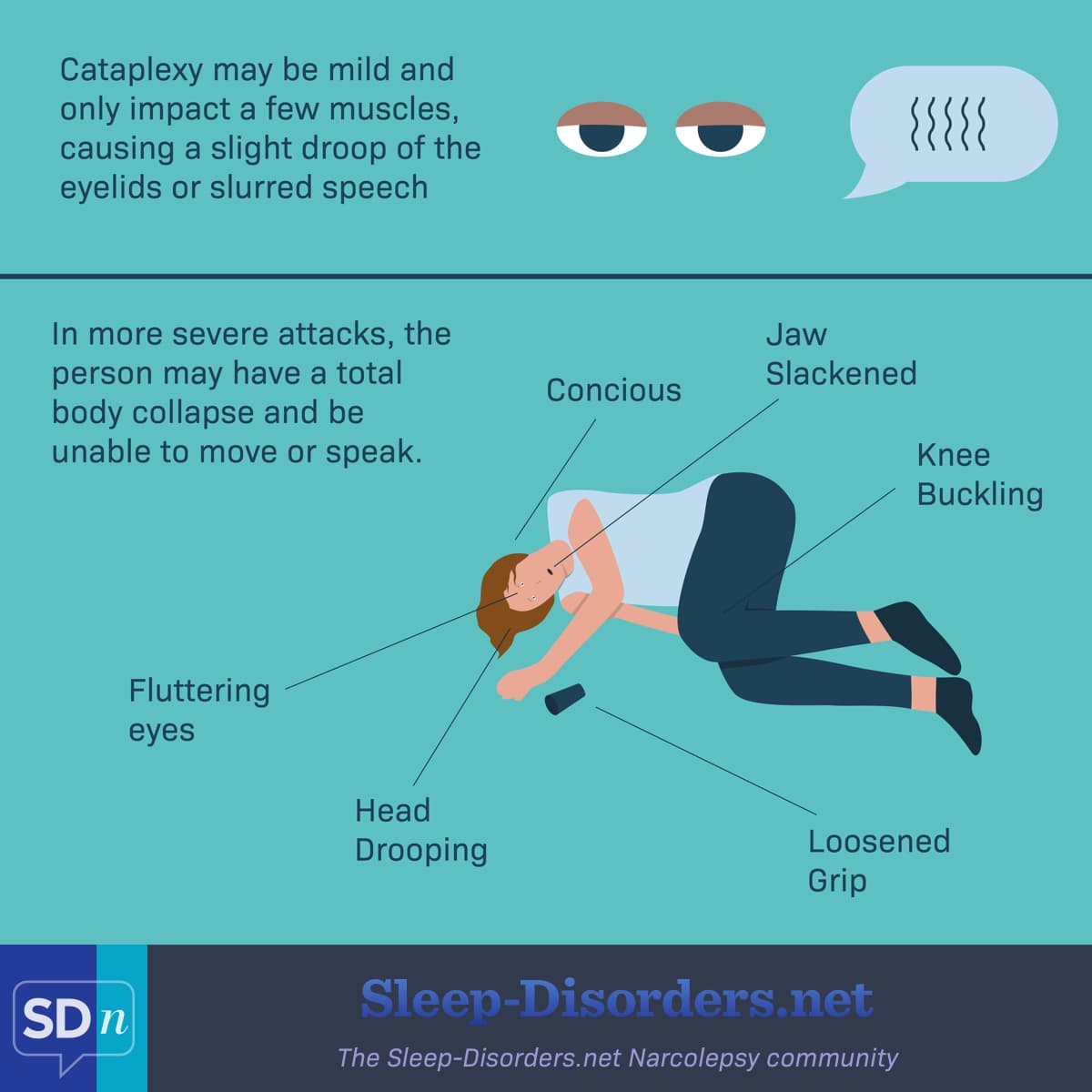
Cataplexy may be mild. It may affect only a few muscles, causing a slight droop of the eyelids or slurred speech. In more severe attacks, a person may have a total body collapse and be unable to move or speak.1,2,4
However, people with cataplexy remain awake and are aware of what is happening around them. They may keep their eyes open throughout an attack.1
Figure 1. What happens to the body during cataplexy
Episodes of cataplexy usually last a few minutes at the most. Some people fall asleep after an attack. Even severe cataplexy by itself is not dangerous, as long as the person can find a safe place to collapse. It can profoundly impact the quality of someone’s life and may prevent them from certain activities such as driving or swimming.1,2
Mild cataplexy may be misdiagnosed as a seizure disorder if the person has no other symptoms of narcolepsy.1
Why does cataplexy happen?
During normal sleep, humans lose muscle tone during the REM stage. In people with narcolepsy, the body has lost its ability to regulate sleep and wake stages. This means the person can fall quickly into a REM state in the middle of the day, losing muscle tone even when they are fully awake.2
How is cataplexy treated?
Not everyone with cataplexy will require medicine but there are several treatment options available. When needed, certain antidepressants may be prescribed, such as:4,5
- Effexor® (venlafaxine)
- Prozac® (fluoxetine)
- Anafranil® (clomipramine)
- Vivactil® (protriptyline)
Xyrem®, Xywav®, or Lumryz™ (sodium oxybate) may be prescribed to treat both daytime sleepiness and cataplexy. These drugs are thought to suppress the brain chemicals, or neurotransmitters, that encourage REM sleep and reduce cataplexy.6-8
Xyrem, Xywav, and Lumryz all have a boxed warning, the strictest warning from the US Food and Drug Administration (FDA). They have this warning because they are central nervous system depressants and can result in coma or death if misused.6-8
Wakix® (pitolisant) is also FDA-approved for the treatment of cataplexy and sleepiness in narcolepsy in adults. It increases histamine levels in the brain and stabilizes sleep.9
Work with a sleep specialist
If you have narcolepsy, it is very important to work with a sleep specialist who can work with you to understand your specific symptoms, concerns, and treatment options that are available to you. Check out this list of accredited sleep specialists around the country. Find one near you for the best care.